A few weeks ago, La Tribune de Genève reported a deeply troubling incident at the University Hospitals of Geneva (HUG): a woman, responsible for patient care, arrived at work to find these words scrawled on her office door: “N****r, get out!!!”
This was not just an insult — it was an act of racial violence that exposes institutional racism and raises urgent questions about workplace culture, patient safety, and the treatment of Black professionals in healthcare.
In this article, I reflect on this case, share my own experience with the “Mediterranean syndrome,” and outline concrete steps hospitals and organisations can take to respond responsibly and build truly inclusive environments.
Read my full piece here ⬇️
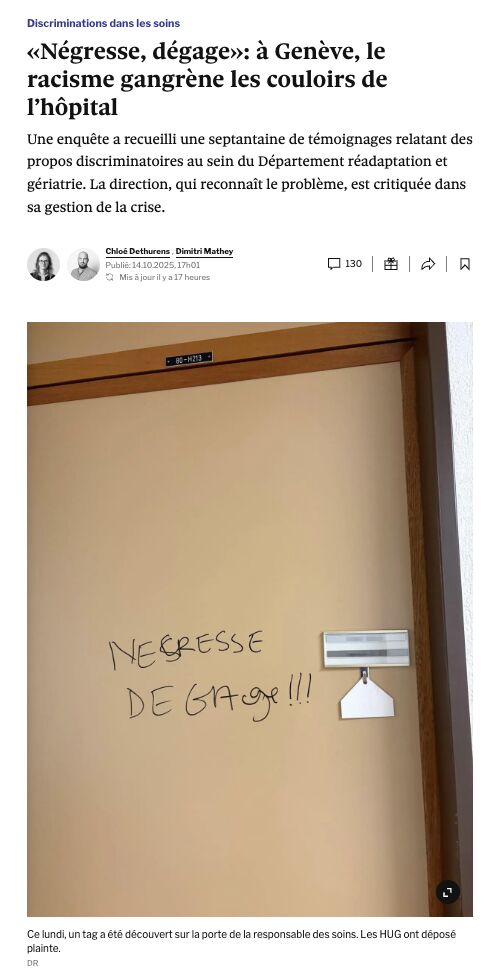
Imagine the scene: you arrive at work and find these words scrawled on your office door:
“N****r, get out!!!”
This is not a mere insult, and its use is far from trivial. It’s a word of unspeakable violence, rooted in the transatlantic slave trade. It carries centuries of exploitation, dehumanisation, and racial hierarchy — a structural injustice that continues to echo through history. On its own, this word constitutes a racist verbal assault, a direct attack on one’s dignity and integrity.
At the University Hospitals of Geneva (HUG), where this incident occurred, the act exposes a deeply troubling form of institutional racism. While the psychological impact on the targeted Patient Care Supervisor is profound, an even greater risk emerges: a racist workforce can compromise patient safety, dignity, and the quality of care.
When employees feel free to express racist views toward their colleagues, it raises a crucial question: how can the institution protect its most vulnerable population — the patients? What remains to prevent these same individuals from reproducing discriminatory behaviours toward those already weakened by illness or trauma?
A hospital should be a sanctuary, a place where humanity stands at the core of every interaction. Racism within its walls is not only unacceptable, it is a betrayal of the very mission of care.
Six urgent actions for a responsible and humane crisis response
1. Public condemnation of the racist attack by leadership
This symbolic gesture is essential: it shows both staff and the public that the institution recognises the seriousness of the act and refuses any form of normalisation. Silence or neutral statements are perceived as passive complicity.
2. Immediate psychological support for the targeted person
The person affected must receive prompt and confidential psychological support. This assistance helps prevent secondary trauma, which often arises from isolation and a lack of institutional recognition.
3. Independent, impartial, and transparent investigation
An internal inquiry conducted by individuals within the same hierarchy undermines the credibility of the process. Involving an external body ensures an objective evaluation, free from conflicts of interest, and strengthens staff trust. The investigation should not only establish the facts but also identify the systemic weaknesses that allowed the incident to occur.
4. Transparent communication throughout the process
Keeping staff informed — without disclosing confidential information — helps prevent rumours, denial, and division. Clear, factual, and empathetic communication rebuilds trust and demonstrates that leadership is acting transparently rather than minimising the issue.
5. Sanctions proportionate to the seriousness of the act
Consequences must match the gravity of the offence: suspension, disciplinary transfer, or dismissal. Sanctions must be applied consistently and fairly, without preferential treatment based on rank or role. Only then can a genuine zero-tolerance culture take root.
6. Mandatory training for all staff in contact with patients on diversity, integrity, and racial bias — including the “Mediterranean syndrome.”
Prevention begins with education. Every professional working with patients should receive training on diversity, racial bias, and respect for integrity, including awareness of the “Mediterranean syndrome.” These reflective spaces help staff understand how unconscious prejudice can unconsciously shape clinical judgment and compromise the quality of care.
Building an inclusive culture of care
The challenge goes far beyond disciplinary action: it is about protecting staff and patient integrity, restoring trust, and preventing future harm. With over 13,000 employees, HUG is a cornerstone of employment in Geneva. Its response will be closely watched. Acting swiftly, with courage and firmness, will send a strong message — to the medical community and beyond.
This is not optional, it’s the condition for turning this crisis into an opportunity to build a hospital that is inclusive and safe for all.
*The “Mediterranean syndrome” refers to an ethno-racial bias observed in medical settings, where patients of African origin are often perceived as exaggerating their pain. This stereotype, unsupported by clinical evidence, leads to the trivialisation of symptoms and unequal treatment. It illustrates how cultural bias can infiltrate the care relationship and compromise the quality of diagnosis and treatment. (Source: Blandenier E., Chollet M., Morisod K., Grazioli V., Dzi K., Bodenmann P. “Racism in health care – Part 3: The Mediterranean syndrome”, Life Science Alliance, 2021.)

